The Pain Academy
Our pain academy is a truly interdisciplinary endeavour that places the individual at its core.
In addition to understanding the biomedical symptoms of pain with reference to the physiology and biochemistry of the body and how it is perceived in the brain, we are also interested in the factors outside of the body that influences how we feel pain. This includes our prior experience with pain, the prevalence of pain in our family, our diet, physical activity, our jobs, the list goes on. We also work as part of multidisciplinary teams to find ways to interact with and mitigate pain. Understanding the pharmacology and behavioural effect of medical interventions such as painkillers is just as important as knowing when to apply more social mediations (like walking and talking therapies). Our aim is to improve knowledge both within healthcare and the public to change the narrative around pain, opening up possibilities for tackling it that have not been considered before.
Some projects we are involved in:
 |
Skills not pills: community-based pain self-management |
|---|
Persistent pain is a huge health challenge. It is the biggest reason people in the UK see their GP. The World Health Organisation (WHO) recognised it as a priority disease in 2019. The National Institute for Health and Care Excellence has also recently accepted that current chronic pain medications have limited use, and in fact carry serious safety concerns. That is why reducing opioid prescriptions (for non-cancer pain) to zero by 2024 is a priority for Public Health England (PHE).
Pain is a bio-psycho-social phenomenon that cuts across social, primary care, public health and rehabilitation. Health care professionals realise the need to change how they engage with people with persistent pain. Persistent pain cannot be ‘fixed’ or ‘cured’. It needs an understanding of the individual experience and person-centred management, to help people live better lives with it. The sustainability of health systems must be re-evaluated. There is potential for families and the community to offer support, and improve the experiences of individual pain-livers. A different way of thinking about health and care in pain management is required.
Durham’s “Skills not pills” approach comprises a ‘Gabapentinoid and Opioid Tapering Toolbox’ (GOTT) and Footsteps App. This offers a set of tools to improve confidence of primary care clinicians and pharmacists and their patients to self-manage chronic pain.
The “Skills not pills” project is supported by our newly launched virtual platform: Footsteps Pain Festival (e-social prescribing), developed, an App under development and hosted by the Live well with pain team and Durham University.
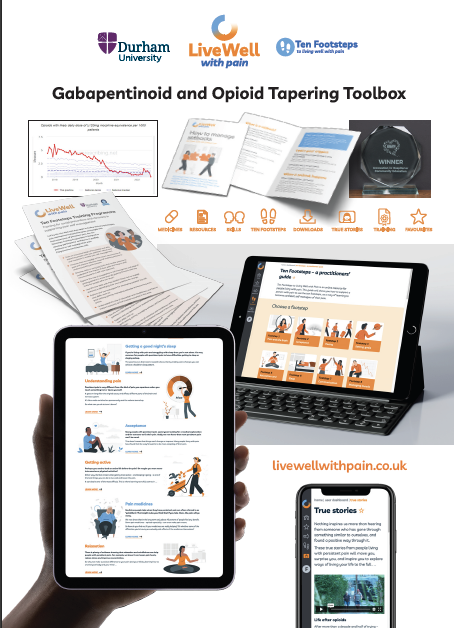
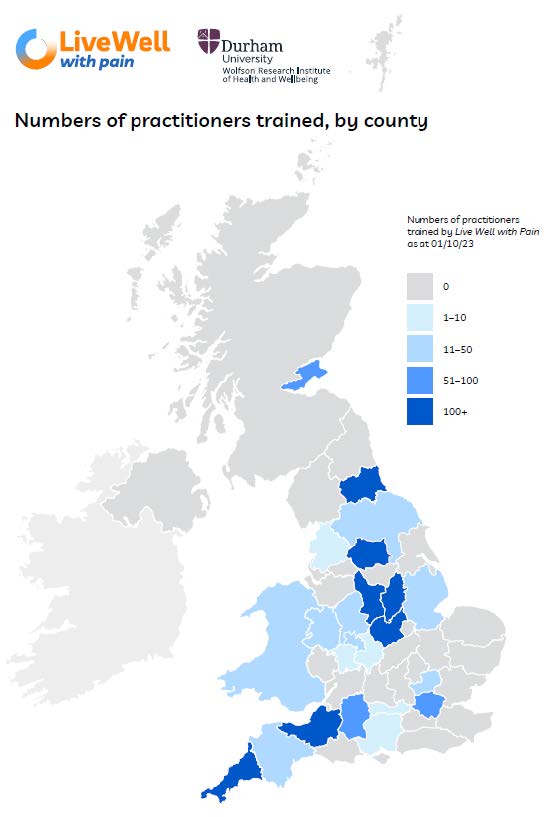
AHSN award-winning LWWP GOTT 10 Footsteps pain self-management Training programme : MAP of impact in UK geographical areas (October 2023)
 |
Rational drug design for managing chronic pain based on the histamine system |
|---|
We are current seriously lacking effective and safe medications for managing chronic pain. We argue that the major efficacy and safety issues with current medications lie in the fact that these can easily access the brain. The Pain academy has focussed on developing medications which are centrally-sparing. Histamine, acting via distinct histamine receptor, regulates various physiological and pathological processes, including chronic pain, in all parts of the body. In the last two decades, there has been a particular increase in evidence to support the involvement of peripheral histamine in the modulation of chronic neuropathic and inflammatory pain, which remains challenging in terms of management. A pair of clinically-ready centrally-sparing drugs, one synthetic and one a natural product, are currently in the final stages of validation for translation to the clinic by the Pain Academy. For the full press release please visit here.
Useful Links and Documents
- INNOVATION HUB - Live Well with Pain
- Making Decisions to help you live well with chronic primary pain
- Fuse award winning unmasking pain project: preliminary findings
- Fuse award winning unmasking pain project: Insights from people with pain, artists, and pain specialists
- Pain CoP 26th September Live Well with Pain webinar
- Unmasking Pain - The Documentary (Youtube Link)
- Living Well with Pain (Julie Ward article in Yorkshire Bylines)
- Chronic Pain: co-production means better health and well-being – confident to support self-management - Recording available here. Please click to access the recording.
- Ten Footsteps for Carers (external page)
- Our Fuse health award winning Unmasking pain project in 5 min (Youtube)
- Chronic Pain: Communication Skills and Self Management PDF (External Page)
- Unmasking Pain Brochure
- GOTT 10-Footsteps Live well with Pain Self-management Programme
- SSM Annual Scientific Meeting September 2023 - Fuse award winning unmasking pain project: Insights from people with pain, artists, and pain specialists
- SSM Annual Scientific Meeting September 2023 - Fuse award winning unmasking pain project: preliminary findings
- Unmasking Pain Academic Poster

Louise’s story
 The lovely Louise Trewern, our Expert Pain Liver lead on the GOTT 10-Footsteps pain self-management training programme and LWWP e-Festival, is co-author on this new article just published by the BMJ. Acknowledging chronic pain as a diagnosis in its own right can help clinicians and patients move on from a mindset of searching for a diagnosis to discussing long term management strategies, Consider non-pain features such as poor sleep, low mood, and reduced physical activity: these can be both a cause and a consequence of chronic primary pain. Consultations where patients feel believed, listened to, and validated can enable a therapeutic relationship that forms the basis for subsequent management strategies, including supported self-management.
The lovely Louise Trewern, our Expert Pain Liver lead on the GOTT 10-Footsteps pain self-management training programme and LWWP e-Festival, is co-author on this new article just published by the BMJ. Acknowledging chronic pain as a diagnosis in its own right can help clinicians and patients move on from a mindset of searching for a diagnosis to discussing long term management strategies, Consider non-pain features such as poor sleep, low mood, and reduced physical activity: these can be both a cause and a consequence of chronic primary pain. Consultations where patients feel believed, listened to, and validated can enable a therapeutic relationship that forms the basis for subsequent management strategies, including supported self-management.
Louise Trewern has lived with pain since childhood. After years of strange illnesses and infections, inconclusive tests and persistent pain, Louise was diagnosed with Fibromyalgia and Osteoarthritis. She was prescribed opioid medication for back pain, which increased over a 13 year period to dangerously high levels, along with a cocktail of other drugs such as antidepressants and benzodiazepines. With support from her local pain service Louise reduced and eventually came off her opioids and learned to self-manage her pain in other ways. She considers that this process literally ‘saved her life.’ Louise today is a very passionate patient-advocate advising The British Pain Society’s Patient Voice Committee where she is Vice Chair. She is on Executive Committee of The Physiotherapy Pain Association and Chair of the Get Involved – Evolving Through Patient Experience Committee at Torbay Hospital Pain Service, as well as numerous other projects including supporting and advising Live Well with Pain. Louise also blogs for Live Well with Pain on our sister site for patients My Live Well with Pain

Unmasking Pain Project - Basis and Early Findings From Sensory Storytelling, Imagination and Wellbeing Project Symposium. Hosted by Leeds University
This video, kindly shared by Paul Chazot, Balbir Singh explores the early findings of the Unmasking Pain Project. This presentation took place at the Sensory Storytelling, Imagination and Wellbeing Project Symposium, hosted by Leeds University, 15 September 2022.


/prod01/prodbucket01/media/durham-university/research-/research-institutes/wolfson-research-institute/60056.jpg)

